If you think that studying the deadly Ebola virus is all about donning a biohazard suit in a high-tech lab, think again. Check out these scientists from the National Institute of Allergy and Infectious Diseases and their collaborators as they travel to a remote village in the Republic of the Congo to search for Ebola and other emerging viruses. Watch them set up camp in the jungle and take blood samples from animals that may harbor these viruses.
Tracking a Deadly Virus
How Influenza Pandemics Occur
| Credit: National Institute of Allergy and Infectious Diseases, NIH |
Flu season is upon us! Check out this NIH video to see how these pandemics emerge and spread new flu viruses around the globe.
Promising Treatment for New Human Coronavirus

Caption: Transmission electron micrograph of novel coronavirus
Credit: Rocky Mountain Laboratories, National Institute of Allergy and Infectious Diseases, NIH
In Fall 2012 a new coronavirus appeared on the global public health radar. The virus has caused 17 cases of severe respiratory disease in the Middle East and Europe, and 11 of these people died. This new virus attracted immediate attention because of the high fatality rate—and because it was in the same family as the virus that caused the global outbreak of severe acute respiratory syndrome (SARS) in 2003, which sickened more than 8,000 people.
A team here at the virus ecology unit at NIAID got a sample of the virus, called nCoV, from The Netherlands in November. By December they had developed an animal model to study how the virus behaved and caused illness. Now, just a few months later, they report that two antiviral drugs, ribavirin and interferon-alpha 2b, will stop nCoV from replicating in cells grown in the lab.
Clearly more studies are needed to figure out whether the treatment will translate to humans, but it’s an important first step. That’s virus to treatment in about four months—pretty impressive.
References:
Inhibition of novel β coronavirus replication by a combination of interferon-α2b and ribavirin. Falzarano D, de Wit E, Martellaro C, Callison J, Munster VJ, Feldmann H. Sci Rep. 2013 Apr 18;3:1686.
Pneumonia from Human Coronavirus in a Macaque Model. Munster VJ, de Wit E, Feldmann H. N Engl J Med. 2013 Apr 18;368(16):1560-1562. Epub 2013 Apr 3.
NIH support: National Institute of Allergy and Infectious Diseases
Eradicating Ebola: In U.S. Biomedical Research, We Trust

Caption: Researcher inside a biosafety level 4 laboratory, which provides the necessary precautions for working with the Ebola virus.
Credit: National Institute of Allergy and Infectious Diseases, NIH
Updated August 28, 2014: Today, the National Institutes of Health (NIH) announced plans to begin initial human testing of an investigational vaccine to prevent Ebola virus disease. Testing of the vaccine, co-developed by NIH’s National Institute of Allergy and Infectious Diseases (NIAID) and GlaxoSmithKline, will begin next week at the NIH Clinical Center in Bethesda, MD.
As the outbreak of Ebola Virus Disease continues to spread in West Africa, now affecting four countries in the region, I am reminded how fragile life is—and how important NIH’s role is in protecting it.
NIH research has helped us understand how Ebola initially infects people and how it spreads from person to person. Preventing this spread is currently our greatest defense in fighting it. Through research, we know that the Ebola virus is transmitted through direct contact with bodily fluids and is not transmitted through the air like the flu. We also know the symptoms of Ebola and the period during which they can appear. This knowledge has informed how we manage the disease. We know that the virus can be contained and eradicated with early identification, isolation, strict infection control, and meticulous medical care.
Research also is helping to develop new strategies against Ebola Virus Disease. Scientists employed and funded by NIAID have been working for decades to develop tests to diagnose the virus early, therapies to treat illness caused by the virus, and vaccines to prevent infection. Several experimental products are in early development and showing promise in laboratory models—a necessary step before testing in humans.
Because of the current situation in Africa, NIAID’s Vaccine Research Center has accelerated an early-stage clinical trial to test the safety of a candidate Ebola vaccine in humans. The trial will start enrolling patients next month. If the vaccine is found to be safe, the trial will move to the next phase to test whether the vaccine produces protective antibodies to fight the virus. This testing could begin as early as January. Optimistically, the vaccine could be available about a year after that for people at highest risk for exposure to Ebola, such as health care workers.
In addition to prevention, research is finding ways to treat the disease. NIH has been supporting the development of a number of promising treatments, including preclinical work on a monoclonal antibody combination that has showed benefit in a monkey model of the disease. A monoclonal antibody is a molecule produced in a lab and engineered to stimulate the immune system to attack an invader, such as a virus or cancer.
You may have seen news reports that two Americans who contracted the virus in Africa and were transported to Emory University Hospital received such a monoclonal antibody treatment as an emergency step, without any certainty whether or not this has helped their recovery. The manufacturer of this experimental treatment continues to research and evaluate the product’s safety and effectiveness. The treatment will have to complete clinical trials to test safety and effectiveness in humans. Even if the Food and Drug Administration authorized the monoclonal antibody product for emergency use, there currently are only a few courses of the treatment available. The product is actually made in tobacco plants, and scale up is a slow and complex process. The product is just one of several supported by NIAID that are showing promise in preclinical testing and are being reviewed for possible scale up and emergency use in West Africa.
At this time, however, the most effective way to stop the current Ebola outbreak in West Africa is meticulous work in finding Ebola cases, isolating and caring for those patients, and tracing contacts to stop the chain of transmission. It requires educating people about safe burial practices and having health care workers strictly follow infection control in hospitals. This is how all previous Ebola outbreaks have been stopped.
We are fortunate to live in a country that places such a high value on biomedical research and public health systems. Through this investment, we protect the health of Americans and people around the world. It is during these times of tragedy that my faith in the U.S. biomedical research enterprise and public health system is especially strong. Together with the leadership of the affected countries in West Africa, the World Health Organization, dedicated medical aid organizations like Doctors Without Borders, and the remarkable efforts of our colleagues at the Centers for Disease Control and Prevention who are ably leading the current U.S. response, we will ultimately contain this outbreak and prevent future ones.
Links:
NIH to Launch Human Safety Study of Ebola Vaccine Candidate, NIAID News Release, 28 August 2014
Understanding Ebola and Marburg hemorrhagic fevers (NIAID)
Tracking a Deadly Virus, NIH Director’s Blog, 14 November 2012
CDC: Stopping the Ebola Outbreak
Using Genomics to Follow the Path of Ebola

Caption: Colorized scanning electron micrograph of filamentous Ebola virus particles (blue) budding from a chronically infected VERO E6 cell (yellow-green).
Credit: National Institute of Allergy and Infectious Diseases, NIH
Long before the current outbreak of Ebola Virus Disease (EVD) began in West Africa, NIH-funded scientists had begun collaborating with labs in Sierra Leone and Nigeria to analyze the genomes and develop diagnostic tests for the virus that caused Lassa fever, a deadly hemorrhagic disease related to EVD. But when the outbreak struck in February 2014, an international team led by NIH Director’s New Innovator Awardee Pardis Sabeti quickly switched gears to focus on Ebola.
In a study just out in the journal Science [1], this fast-acting team reported that it has sequenced the complete genetic blueprints, or genomes, of 99 Ebola virus samples obtained from 78 patients in Sierra Leone. This new genomic data has revealed clues about the origin and evolution of the Ebola virus, as well as provided insights that may aid in the development of better diagnostics and inform efforts to devise effective therapies and vaccines.
To help advance such research, Sabeti’s team deposited its Ebola genome sequences, even prior to publication, in a database run by NIH’s National Center for Biotechnology Information’s (NCBI), which means the data is immediately and freely available to researchers around the world. Access to this genomic data should accelerate international efforts to figure out ways of detecting, treating, and, ultimately, preventing infection by this deadly virus.
Sophisticated genomic analyses by Sabeti and her colleagues show that the current Ebola Virus Disease outbreak most likely originated less than a year ago with a single person, starting at the funeral of a traditional healer in Guinea and eventually spreading to Sierra Leone and other nations. In contrast, previous EVD outbreaks appear to have been fueled primarily by humans being directly exposed to infected fruit bats or other animals harboring the virus. These findings underscore the need to take proper precautions, as outlined by the Centers for Disease Control and Prevention, to prevent the spread of the virus from human to human.
As for possible implications of this work for diagnosis and treatment, Sabeti’s team found that the Ebola virus strain (EBOV) responsible for the 2014 outbreak in West Africa appears to have evolved from a strain that caused an outbreak in Central Africa in 2004, with changes occurring in nearly 400 regions of the genome. These findings are important, because some of the tests currently used to diagnose EBOV might fail to work in the presence of these genetic changes—meaning they could give false negative test results in some people who are actually infected with the virus. Now, thanks to Sabeti’s genomic profiling of EBOV, it should be possible to enhance diagnostic tests to pick up nearly all forms of the virus. Continued genomic sequencing will be critical to keep the diagnostics up-to-date, because the Ebola virus will continue to evolve over the course of the outbreak.
Sabeti, who is a computational geneticist at the Broad Institute of Harvard and MIT in Cambridge, MA, says among the urgent questions still to be answered is whether these genetic changes might influence the speed at which the virus spreads or the severity of the disease it causes.

Caption: In Memory of Sheik Humarr Khan, who was part of the research team that sequenced the Ebola Virus genome. Dr. Khan died from Ebola Virus Disease while overseeing patient care at Kenema Government Hospital in Sierra Leone.
Credit: Pardis C. Sabeti
As of August 28, the Ebola virus outbreak in West Africa has infected at least 3,069 people and killed 1,552 [2], making it the largest outbreak on record since the disease was first identified in 1976. Sadly, among its victims were five members of Sabeti’s team who died before their paper was published, including Dr. Sheik Humarr Khan, a leading virologist in Sierra Leone.
So, let me close by paying tribute to these brave researchers—and all of the other dedicated scientists and healthcare workers on the front lines of the Ebola Virus Disease epidemic and other public health emergencies around the globe. You bring both comfort and hope to those who need it the most. From all of us here at NIH, let me convey our gratitude for your dedication.
References:
[1] Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Gire SK, Sabeti PC, et al. Science (published online August 28, 2014)
[2] Ebola virus disease update—West Africa (WHO)
Links:
Emerging Disease or Emerging Diagnosis? (NIH Common Fund Video Competition)
Understanding Ebola and Marburg hemorrhagic fevers (NIAID)
Ebola Hemorrhagic Fever, Prevention (CDC)
CDC: Stopping the Ebola Outbreak
NIH support: Common Fund, National Institute of Allergy and Infectious Diseases
Vaccine Research: New Tactics for Tackling HIV
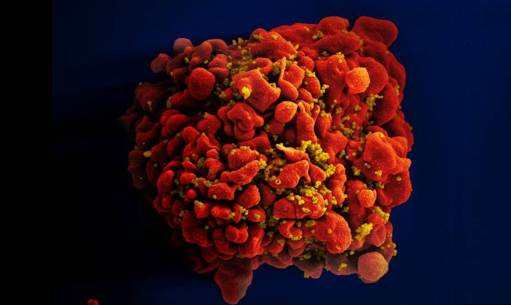
Caption: Scanning electron micrograph of an HIV-infected immune cell.
Credit: National Institute of Allergy and Infectious Diseases, NIH
For many of the viruses that make people sick—think measles, smallpox, or polio—vaccines that deliver weakened or killed virus encourage the immune system to produce antibodies that afford near complete protection in the event of an exposure. But that simple and straightforward approach doesn’t work in the case of human immunodeficiency virus (HIV), the virus that causes AIDS. In part, that’s because our immune system is poorly equipped to recognize HIV and mount an attack against the infection. To make matters worse, HIV has a habit of quickly mutating as it multiplies.That means, in order for an HIV vaccine to be effective, it must induce antibodies capable of fighting against a wide range of HIV strains. For all these reasons, the three decades of effort to develop an HIV vaccine have turned out to be enormously challenging and frustrating.
But now I’m pleased to report that NIH-funded scientists have taken some encouraging strides down this path. In two papers published in Science [1, 2] and one in Cell [3], researchers presented results of animal studies that support what most vaccine experts have come to suspect: the immune system is in fact capable of producing the kind of antibodies that should be protective against HIV, but it takes more than one step to get there. In effect, a successful vaccine strategy has to “take the immune system to school,” and it requires more than one lesson to pass the final exam. Specifically, what’s needed seems to be a series of shots—each consisting of a different engineered protein designed to push the immune system, step by step, toward the production of protective antibodies that will work against virtually all HIV strains.
The new work builds upon basic research discoveries made over the last decade showing that some people infected with HIV eventually do develop a strong immune response that is characterized by broadly neutralizing antibodies (bnAbs) [4 – 6]. Unfortunately, this response appears only in a minority of people infected with HIV, after years of attack and counterattack between the virus and those individuals’ immune systems. Since those discoveries, vaccine researchers have been busy trying to figure out how to mimic this natural effect in a swifter and more reliable manner that would enable uninfected people to produce bnAbs that could ward off HIV infection.
What makes bnAbs special are their unusual features, which allow them to bind to certain parts of spiky proteins found on the surface, or envelope, of HIV. Unlike many other parts of HIV, these binding sites are “conserved”—which means they don’t change frequently. Researchers regard conserved areas of a virus as ideal targets for the development of vaccines that provide broad, long-lasting protection.
However, a major challenge for HIV vaccine development is that the human genome doesn’t directly code for bnAbs with the ability to bind the virus at its most conserved—and, consequently, most vulnerable—locations. Rather, the development of such bnAbs hinges upon the ability of the antibody genes of certain B cells (a type of white blood cell involved in immune response) to go through a series of DNA rearrangements and mutations, producing precursor proteins that gradually adapt and change over time into bnAbs capable of neutralizing HIV in its many forms.
In one of the new studies, a team led by David Nemazee, William Schief, and Dennis Burton at The Scripps Institute, La Jolla, CA, reported that it may be possible to optimize bnAb production with a protein nanoparticle specifically engineered to activate the B cells that produce bnAb precursors. In experiments involving a line of mice genetically modified to produce human-like antibodies, the researchers found immunization with an engineered HIV envelope protein, called eOD-GT8 60mer, spurred production of antibodies with some—but not all—of the traits necessary to recognize and block HIV infection. This finding suggests that eOD-GT8 60mer or a similar engineered protein may be a good candidate to serve as the first in a series of immunizations against HIV.
In the second study, a team led by John P. Moore and Rogier Sanders of Weill Medical College of Cornell University, New York, tested the powers of a protein engineered to mimic a highly conserved region of HIV’s envelope proteins.Using rabbit and macaque models, the researchers showed that this protein does elicit an immune response against HIV. Like the protein used in the first study, it did not generate the full neutralizing coverage needed to provide effective protection against a wide range of HIV strains. Still, these findings indicate that one or more proteins designed to mimic this highly conserved portion of HIV should be considered for inclusion in sequential approaches to HIV immunization.
Last but certainly not least, a team led by Schief and Michel Nussenzweig at The Rockefeller University, New York, published a paper that pulls together both new pieces of the HIV vaccine puzzle. Using a different strain of mice, these researchers confirmed that the eOD-GT8 60mer protein does indeed activate the right kind of B cells to get an immune response going. Their experiments in another strain of mice genetically modified to represent a later stage of infection also confirmed that in order to keep the immune response rolling toward truly effective HIV protection, other proteins engineered to mimic HIV envelope proteins will likely be needed. Taken together, these findings provide much-needed, experimental support for the notion that the best bet for an effective HIV vaccine may lie in a strategic sequence of immunizations, each guiding the immune system towards the production of bnAbs.
With about 50,000 Americans and more than 2 million people worldwide becoming newly infected with HIV every year [7], it’s clear that the quest for effective HIV vaccines and treatments has to be a top research priority. There’s a lot of work that still must be done before we can test this sequential HIV vaccine approach in humans, but—as these three new studies show—it looks like science is on a promising new track.
References:
[1] Priming a broadly neutralizing antibody response to HIV-1 using a germline- targeting immunogen. Jardine JG, Ota T, Sok D, Pauthner M, Kulp DW, Kalyuzhniy O, Skog PD, Thinnes TC, Bhullar D, Briney B, Menis S, Jones M, Kubitz M, Spencer S, Adachi Y, Burton DR, Schief WR, Nemazee D. Science. 2015 Jun 18. [Epub ahead of print]
[2] HIV-1 neutralizing antibodies induced by native-like envelope trimers. Sanders RW, van Gils MJ, Derking R, Sok D, Ketas TJ, Burger JA, Ozorowski G, Cupo A, Simonich C, Goo L, Arendt H, Kim HJ, Lee JH, Pugach P, Williams M, Debnath G, Moldt B, van Breemen MJ, Isik G, Medina-Ramírez M, Back JW, Koff WC, Julien JP, Rakasz EG, Seaman MS, Guttman M, Lee KK, Klasse PJ, LaBranche C, Schief WR, Wilson IA, Overbaugh J, Burton DR, Ward AB, Montefiori DC, Dean H, Moore JP. Science. 2015 Jun 18. [Epub ahead of print]
[3] Immunization for HIV-1 broadly neutralizing antibodies in human Ig knockin mice. Dosenovic P, von Boehmer L, Escolano A, Jardine J, Freund NT, Gitlin AD, McGuire AT, Kulp DW, Oliveira T, Scharf L, Pietzsch J, Gray MD, Cupo A, van Gils MJ, Yao KH, Liu C, Gazumyan A, Seaman MS, Björkman PJ, Sanders RW, Moore JP, Stamatatos L, Schief WR, Nussenzweig MC. Cell. 2015 Jun 18;161(7):1505-15.
[4] Broadly neutralizing antibodies and the search for an HIV-1 vaccine: the end of the beginning. Kwong PD, Mascola JR, Nabel GJ. Nat Rev Immunol. 2013 Sep;13(9):693-701.
[5] Broadly neutralizing antibodies and the development of vaccines. Haynes BF, Bradley T. JAMA. 2015 Jun 23-30;(24):2419-2420.
[6] The modern era of HIV-1 vaccine development. Mascola JR. Science 2015 Jul 10;349(6244):139-140.
[7] HIV/AIDS: Basic Statistics. Centers for Disease Control and Prevention. May 11, 2015.
Links:
HIV Vaccine Research (National Institute of Allergy and Infectious Diseases/NIH)
Center for HIV/AIDS Vaccine Immunology & Immunogen Discovery (The Scripps Institute, LaJolla, CA)
Michel Nussenzweig (The Rockefeller University, New York)
John P. Moore (Weill Cornell Medical College, New York)
NIH Support: National Institute of Allergy and Infectious Diseases; National Center for Advancing Translational Sciences
Snapshots of Life: New Target for Herpes Treatment?
 Something about this image reminds me of that wacky and infectious old song: “It was a one-eyed, one-horned, flyin’ purple people eater …” Of course, this purple blob isn’t a people eater, but it does happen to be infectious. What you see here is a 3D rendering of a protein that the herpes simplex virus 1 (HSV-1)—one of two herpes viruses that cause genital herpes and cold sores—depends upon to infect human cells.
Something about this image reminds me of that wacky and infectious old song: “It was a one-eyed, one-horned, flyin’ purple people eater …” Of course, this purple blob isn’t a people eater, but it does happen to be infectious. What you see here is a 3D rendering of a protein that the herpes simplex virus 1 (HSV-1)—one of two herpes viruses that cause genital herpes and cold sores—depends upon to infect human cells.
When a cell is infected with HSV-1, the virus inserts its DNA into human cells, periodically coming out of dormancy to make more copies of itself. However, errors sometimes occur when the DNA is replicated. When that happens, an HSV-1 protein, dubbed infected cell protein 8 (ICP8), stitches broken pieces of DNA back together. That’s what you see depicted in this schematic, which shows two single strands of DNA (red with multicolor bases) entering an ICP8 complex (purplish blue) to be reannealed into DNA’s familiar double-stranded helix (red).
It’s important to keep in mind that scientists don’t yet know exactly how ICP8 reassembles DNA. This image, which is one of the winners of the Federation of American Societies for Experimental Biology’s 2014 BioArt competition, models just one potential mechanism. Still, it’s an impressive achievement.
Now a postdoctoral fellow at NIH’s National Cancer Institute, Gökhan Tolun produced this image while in Jack Griffith’s lab at the University of North Carolina, Chapel Hill. Tolun started with many 2D electron microscope images of HSV-1 bound to DNA (those are the very small structures you can see in the background) and used them to generate the 3D structure via sophisticated computational analyses. If you’d like to see more of Tolun’s work, check out this very cool animation that depicts another possible mode of ICP8-mediated DNA repair.
Once infected, human cells aren’t able to rid themselves of herpes virus. Treatments can help prevent outbreaks of symptoms, but there currently is no cure for the more than 750,000 Americans infected with herpes every year. Researchers think ICP8 may prove to be a useful new target for fighting herpes. So, the models that Tolun and his colleagues have created are not only are striking pieces of scientific art—they offer promising molecular insights for all who await new anti-viral strategies.
Links:
Genital Herpes – CDC Fact Sheet (Centers for Disease Control and Prevention)
Griffith Lab (University of North Carolina, Chapel Hill)
BioArt (Federation of American Societies for Experimental Biology, Bethesda, MD)
NIH Support: National Cancer Institute; National Institute of General Medical Sciences; National Institute of Environmental Health Sciences
Zika Virus: An Emerging Health Threat
Credit: Kraemer et al. eLife 2015;4:e08347
For decades, the mosquito-transmitted Zika virus was mainly seen in equatorial regions of Africa and Asia, where it caused a mild, flu-like illness and rash in some people. About 10 years ago, the picture began to expand with the appearance of Zika outbreaks in the Pacific islands. Then, last spring, Zika popped up in South America, where it has so far infected more than 1 million Brazilians and been tentatively linked to a steep increase in the number of babies born with microcephaly, a very serious condition characterized by a small head and brain [1]. And Zika’s disturbing march may not stop there.
In a new study in the journal The Lancet, infectious disease modelers calculate that Zika virus has the potential to spread across warmer and wetter parts of the Western Hemisphere as local mosquitoes pick up the virus from infected travelers and then spread the virus to other people [2]. The study suggests that Zika virus could eventually reach regions of the United States in which 60 percent of our population lives. This highlights the need for NIH and its partners in the public and private sectors to intensify research on Zika virus and to look for new ways to treat the disease and prevent its spread.
Zika virus infection can be spread by yellow fever mosquitoes (Aedes aegypti), and experimental evidence suggests the virus also can be transmitted by Asian tiger mosquitoes (Aedes albopictus). Aedes mosquitoes—already known for transmitting other viral illnesses, such as dengue and chikungunya—have a wide and expanding global distribution, including in the United States [3]. To predict places around the world where Zika virus might spread as people infected in the Brazilian outbreak come into contact with biting Aedes mosquitoes, the NIH-supported research team, led by Kamran Khan of St. Michael’s Hospital, Toronto, first mapped the global distribution of Aedes mosquitoes along with the climate conditions the researchers deemed favorable to the spread of Zika virus. They then layered onto this map the final destinations of travellers who might have been exposed to Zika virus before departing Brazil from September 2014 to August 2015.
During the year, 9.9 million travelers left 146 Brazilian airports near areas known to be conducive to Zika virus transmission for destinations around the world. North and South American countries were the most-popular destinations (representing 65 percent of travelers) followed by those in Europe (27 percent) and Asia (5 percent). The most-popular travel spot was the United States, with more than 2.7 million people making the trip.
According to the researchers’ calculations, about 200 million Americans—more than 60 percent of the population—reside in areas of the United States that might be conducive to the spread of Zika virus during warmer months through biting mosquitoes, including areas along the East and West Coasts and much of the Midwest. In addition, another 22.7 million people live in humid, subtropical parts of the country that might support the spread of Zika virus all year round, including southern Texas and Florida. Already, there are reports of local spread of the virus within Puerto Rico and of travelers returning to the U.S. with the Zika infection.
With all this in mind, it is now critically important to confirm, through careful epidemiological and animal studies, whether or not a causal link exists between Zika virus infections in pregnant women and microcephaly in their newborn babies. Brazilian health authorities made the initial connection between the virus and birth defects, primarily because the increase in microcephaly seemed to emerge a few months after the introduction of Zika virus into Brazil. Thousands of cases of microcephaly have now been reported and the Brazilian health ministry has confirmed the presence of Zika virus in tissue samples and amniotic fluid collected from a small number of affected children or their mothers [1]. While the U.S. Centers for Disease Control and Prevention (CDC) has obtained similar findings, it remains unclear what other factors might increase risks to the developing fetus [4].
In November, health authorities in French Polynesia also reported an unusual increase of central nervous system malformations in fetuses and infants that seemed to coincide with the Zika outbreak there. And, last week, came news reports of the first child born in the U.S. with microcephaly possibly linked to Zika. The child’s mother had lived in Brazil during her pregnancy before moving to Oahu, Hawaii [5]. As an additional concern, there are reports in French Polynesia and Brazil of a possible connection between Zika infection and Guillain-Barré syndrome, a mysterious condition in which the immune system attacks part of the peripheral nervous system [1].
With no vaccine or treatment currently available to prevent or treat Zika infection, the best way for individuals—and pregnant women in particular—to protect themselves is to avoid traveling to places where Zika is known to be spreading. If an individual has to live or work in such a region, CDC recommends strict precautions to avoid mosquito bites, including wearing protective clothing, using insect repellants, and sleeping in rooms with window screens or air conditioning. Though still unproven, the link between Zika infection and microcephaly has also prompted CDC to issue interim guidelines recommending that women who are pregnant or planning to become pregnant consider postponing travel to areas where Zika virus has spread. This frequently updated list currently includes Puerto Rico, Mexico, and 20 other countries in South America, Central America, the Caribbean, the Pacific islands, and Africa [6].
Many important questions remain about Zika. But, as Anthony Fauci, director of NIH’s National Institute for Allergy and Infectious Diseases, noted in his recent New England Journal of Medicine essay, one thing is very clear: far more research into Zika virus and its interactions with its mosquito, human, and non-human primate hosts is urgently needed [7]. For instance, it will be important to determine how readily Asian tiger mosquitoes, which can tolerate relatively cold temperatures, spread Zika virus.
The scientific community must also step up its efforts to develop innovative approaches against the virus, and that’s certainly happening at NIH. With NIAID taking the lead, research is underway to understand better Zika’s effects on the body, to develop diagnostic tests to identify the virus rapidly in people, and to ramp up testing of therapeutics that might be effective. Importantly, NIAID researchers already are working on vaccine candidates to prevent Zika virus from infecting people. All of this work is a compelling example of NIH mobilizing swiftly in the face of a rapidly emerging infectious disease, and seeking the research answers that Americans and people across the globe need.
References:
[1] Rapid risk assessment: Zika virus epidemic in the Americas: potential association with microcephaly and Guillian-Barre syndrome. European Centre for Disease Prevention and Control. 10 December 2015.
[2] Anticipating the international spread of Zika virus from Brazil. Bogoch II, Brady OJ, Kraemer MU, German M, Creatore MI, Kulkarni MA, Brownstein JS, Mekaru SR, Hay SI, Groot E, Watts A, Khan K. Lancet. 2016 Jan 14. pii: S0140-6736(16)00080-5.
[3] The global distribution of the arbovirus vectors Aedes aegypti and Ae. albopictus. Kraemer MU, Sinka ME, Duda KA, Mylne AQ, Shearer FM, Barker CM, Moore CG, Carvalho RG, Coelho GE, Van Bortel W, Hendrickx G, Schaffner F, Elyazar IR, Teng HJ, Brady OJ, Messina JP, Pigott DM, Scott TW, Smith DL, Wint GR, Golding N, Hay SI. Elife. 2015 June 30;4:e08347.
[4] CDC Telebriefing: Zika Virus Travel Alert. Centers for Disease Control. 15 January 2016.
[5] Hawaii baby born with small head had prior Zika infection. CNN. 19 January 2016.
[6] Interim Guidelines for Pregnant Women During a Zika Virus Outbreak — United States, 2016. Centers for Disease Control. 19 January 2016.
[7] Zika Virus in the Americas – Yet Another Arbovirus Threat. Fauci AS, Morens DM. N Engl J Med. 2016 Jan 13. [Epub ahead of print]
Links:
Zika Virus Infection and Pregnancy (CDC)
Kamran Khan (St. Michael’s Hospital, Toronto)
Fogarty International Center (NIH)
NIH Support: Fogarty International Center
Zika Vaccine: Two Candidates Show Promise in Mice

Caption: Zika virus (red), isolated from a microcephaly case in Brazil. The virus is associated with cellular membranes in the center.
Credit: NIAID
Last February, the World Health Organization declared a public health emergency over concerns about very serious birth defects in Brazil and their possible link to Zika virus. But even before then, concerns about the unprecedented spread of Zika virus in Brazil and elsewhere in Latin America had prompted NIH-funded scientists to step up their efforts to combat this emerging infectious disease threat. Over the last year, research aimed at understanding the mosquito-borne virus has progressed rapidly, and we now appear to be getting closer to a Zika vaccine.
In a recent study in the journal Nature, researchers found that a single dose of either of two experimental vaccines completely protected mice against a major viral strain responsible for the Zika outbreak in Brazil [1]. Caution is certainly warranted when extrapolating these (or any other) findings from mice to people. But, taking into account the fact that researchers have already developed safe and effective human vaccines for several related viruses, the new work represents a very encouraging milestone on the road toward a much-needed Zika vaccine for humans.
The two experimental vaccines undergoing testing represent different approaches to vaccine development. One approach, developed by Dan Barouch of Beth Israel Deaconess Medical Center, Boston, and colleagues, is a DNA vaccine composed of select snippets of genetic material from a Zika strain from Brazil. The DNA included in the vaccine encodes proteins found at the viral surface that are known to induce an immune response.
Barouch and his colleagues found that a single shot of their experimental DNA vaccine could induce the production of Zika-specific neutralizing antibodies in mice. To find out whether those antibodies protected against Zika infection, they intravenously delivered live Zika virus from Brazil or Puerto Rico to mice four weeks after receiving either the vaccine or a sham shot.
Unvaccinated mice developed high levels of Zika virus that lasted about six days. In contrast, vaccinated mice showed no detectable Zika virus in their bloodstream. This was, of course, very encouraging news, demonstrating that the vaccine offered complete protection against Zika strains from both Brazil and Puerto Rico. The other good news is the vaccinated mice resisted infection for at least eight weeks.
The second vaccine, developed by a team at the Walter Reed Army Institute of Research, Silver Spring, MD, working in close collaboration with the NIH’s National Institute of Allergy and Infectious Diseases (NIAID), was produced from a purified, inactivated Zika virus from Puerto Rico. To find out whether this vaccine offered similar protection, the researchers assessed whether it was able to induce antibodies that can protect against Zika infection. The results were positive. It will now be important to follow the animals in the coming months to assess how long Zika immunity lasts and test the vaccines in larger animals and in humans.When it comes to vaccine development, multiple options are always best. Purified, inactivated virus vaccines, such as used to develop the annual flu shot, represent a more traditional approach. But DNA vaccines, where the DNA is injected into muscle and directs the production of the relevant antigen, can offer some potential advantages. While no DNA vaccine has yet received FDA approval for human use, there is great interest in introducing this “vaccine of the future” into practice. To produce such vaccines, labs don’t have to grow large batches of virus, which can take time and money. Furthermore, these vaccines allow scientists to include only selected bits of a virus known to produce the desired immune response, with essentially zero risk of inducing an active infection.
At least two other Zika DNA vaccines under development at NIAID and elsewhere are showing promise. The NIAID will launch its first human vaccine safety tests of a DNA vaccine, involving about 80 volunteers, at the end of the summer or in the early fall. The tests will last about three months and should set the stage for a clinical trial to evaluate whether the vaccine guards against Zika infection in people.
This fall, NIAID and Walter Reed plan to launch two clinical trials of inactivated viral vaccines, including the one described in the Nature study. The trials, each involving dozens of volunteers, will test to see whether the vaccines are safe and elicit an immune response in people.
Vaccine development and testing take time. But given the rapid pace of progress, there’s now good reason for hope that a Zika vaccine could be a possibility in the not too distant future.
Reference:
[1] Vaccine protection against Zika virus from Brazil. Larocca RA, Abbink P, Peron JP, Zanotto PM, Iampietro MJ, Badamchi-Zadeh A, Boyd M, Ng’ang’a D, Kirilova M, Nityanandam R, Mercado NB, Li Z, Moseley ET, Bricault CA, Borducchi EN, Giglio PB, Jetton D, Neubauer G, Nkolola JP, Maxfield LF, Barrera RA, Jarman RG, Eckels KH, Michael NL, Thomas SJ, Barouch DH. Nature. 2016 Jun 28. [Epub ahead of print]
Links:
Zika Virus Vaccine Research (National Institute of Allergy and Infectious Diseases/NIH)
Zika Virus (Centers for Disease Control and Prevention)
Zika Virus and Complications (World Health Organization)
Barouch Laboratory (Beth Israel Deaconess Medical Center, Boston)
NIH Support: National Institute of Allergy and Infectious Diseases
Summer Reading Suggestions from Scientists: Robert Horvitz
 Two Science Selections:
Two Science Selections:
Horace Freeland Judson, Eighth Day of Creation. A comprehensive history of the origins and early science of the field of modern molecular biology, written by historian Horace Freeland Judson based on personal interviews with those who drove the revolution in biology. First and foremost are the science—DNA, RNA and protein, the genetic code, and gene regulation—and the scientific process—the seed ideas, the “aha” insights and the brilliant and elegant experiments. But this book is also the story of scientists in the process of discovery and of how the science that emerged was at least as much a consequence of the personalities as of the experimental skills of those involved. Fascinating, engaging, and fun—I’ve recommended this book to many, scientist and non-scientist alike.
Georgina Ferry, Dorothy Hodgkin. A superb biography of one of modern science’s most exceptional and distinguished pioneers. Awarded the Nobel Prize in Chemistry in 1964 for determining the crystal structures of penicillin and vitamin B12, Dorothy Crowfoot Hodgkin faced repeated challenges as a woman attempting to study and then pursue a career in chemistry in the 1930s and 1940s in England. Hodgkin is only one of four women ever awarded the Nobel Prize in Chemistry; the others were Marie Curie (1911); her daughter Irene Joliot-Curie (1935); and Ada Yonath (2009). Once recognized, Hodgkin worked hard to combat social inequalities and was president for more than a decade of Pugwash, an international organization founded by Bertrand Russell and dedicated to preventing war. Hodgkin has been a role model for many, although she disagreed rather strongly with the political views and actions of her most famous student, Margaret Thatcher.
Personal Connection:
George Klein, The Atheist and the Holy City. This book was a gift to me from George Klein, a Hungarian-Swedish tumor biologist and virologist at the Karolinska Institute in Stockholm. George and his wife Eva are best known in biological circles for their pioneering discovery of the role of the Epstein-Barr virus in Burkitt’s lymphoma and other neoplasms. This book, one of many George has written, is a compilation of essays that focus on science, but incorporate history, religion and philosophy. Its sections are entitled “The Wisdom and Folly of Scientists,” “Journeys,” “Viruses and Cancer” and “The Human Condition,” and collectively touch upon topics as diverse as DNA hybridization, the discovery of Rous sarcoma virus, and the life cycle of Schistosoma mansoni, as well as the Nazi death camps, scientific creativity, and the conviction that God is an example of man’s wishful thinking. Thought-provoking and uplifting, this book is a story of science and much more. A must read for all.
Robert Horvitz, Ph.D. is the David H. Koch Professor of Biology at the Massachusetts Institute of Technology, and a member of the MIT McGovern Institute for Brain Research and the MIT Koch Institute for Integrative Cancer Research. Dr. Horvitz is co-winner of the 2002 Nobel Prize in Physiology or Medicine for discoveries concerning genetic regulation of organ development and programmed cell death.
Feed a Virus, Starve a Bacterium?

Thinkstock/Stockbyte
Yes, the season of colds and flu is coming. You’ve probably heard the old saying “feed a cold and starve a fever.” But is that sound advice? According to new evidence from mouse studies, there really may be a scientific basis for “feeding” diseases like colds and flu that are caused by viruses, as well as for “starving” certain fever-inducing conditions caused by bacteria.
In the latest work, an NIH-funded research team found that providing nutrition to mice infected with the influenza virus significantly improved their survival. In contrast, the exact opposite proved true in mice infected with Listeria, a fever-inducing bacterium. When researchers forced Listeria-infected mice to consume even a small amount of food, they all died.
Just like humans, when mice and other mammals come down with many infectious illnesses, they often lose their appetites and shun food. In the new study reported in the journal Cell, a team led by Ruslan Medzhitov, a Howard Hughes Medical Institute Investigator at Yale University School of Medicine, New Haven, CT, and former Lurie Prize winner from the Foundation for NIH, set out to explore how the presence or lack of nutrition might influence recovery from infections [1].
In one series of experiments, the researchers infected mice with the influenza virus, which caused potentially life-threatening bouts of the flu. As expected from past observations, the flu-sickened mice reduced their food intake. However, when the researchers pumped more nutrition into some of the sick mice via tube feeding, their odds of survival were significantly better than those who weren’t given the extra nutrition. Further analysis showed that the animals’ survival appeared to hinge on the availability of glucose. When mice suffering from the flu were starved of glucose, they eventually lost the vital ability to control their body temperatures, breathing, and/or heart rates.
Researchers found the situation to be dramatically different in mice that were infected with the bacterium Listeria, an occasional cause of food poisoning in humans. When mice are sickened by Listeria, they tend to stop eating for a while, before eventually resuming eating and recovering. However, in contrast to mice with the flu virus, when researchers gave the Listeria-infected mice even a small amount of nutrition, all the animals died. Again, it was all about sugar. Glucose alone, delivered via tube feeding or injection, was enough to kill Listeria-infected mice. The cause of death wasn’t an inability to clear the infection: they died from changes to their metabolism that made things worse.
PET scans of mice suffering from viral versus bacterial inflammation also revealed significant differences in the way their brains took up glucose. Taken together, these findings suggest that, by taking advantage of key metabolic differences, nutrition (or lack thereof!) may play an important role in helping mammals mount successful responses to different types of infections, just as the old “feed a cold, starve a fever” adage implies.
In light of the findings in mice, a much closer look may be needed to determine what constitutes optimal nutrition for people dealing with a wide range of infectious illnesses. Medzhitov says he and his colleagues are now in the planning stages for a human clinical trial designed to explore that very issue.
So, what to do if you or a loved one comes down with a cold, the flu, or another viral bug this season? Medzhitov wisely hesitates to provide medical advice, noting that mice are not humans and the findings need to be replicated and confirmed in people. But, in the meantime, it appears that giving the patient with a typical viral syndrome a bowl of ice cream or another glucose-rich treat probably wouldn’t hurt—and might even help. Just be sure first that it’s not a serious bacterial infection.
References:
[1] Opposing effects of fasting metabolism on tissue tolerance in bacterial and viral inflammation. Wang A, Huen SC, Luan HH, Yu S, Zhang C, Gallezot JD, Booth CJ, Medzhitov R.Cell.2016 Sep 8;166:1-14.
Links:
Ruslan Medzhitov (Yale University School of Medicine, New Haven, CT)
NIH Support: National Institute of Allergy and Infectious Diseases; National Cancer Institute; National Institute of Arthritis and Musculoskeletal and Skin Diseases; National Institute of Diabetes and Digestive and Kidney Diseases
Simplifying HIV Treatment: A Surprising New Lead

Caption: PET/CT imaging reveals a surprisingly high concentration (yellow, light green) of key immune cells called CD4 T cells in the colon (left) of an SIV-infected animal that received antibody infusions along with antiviral treatment. Fewer immune cells were found in the small intestine (right), while the liver (lower left) shows a high level of non-specific signal (orange).
Credit: Byrareddy et al., Science (2016).
The surprising results of an animal study are raising hopes for a far simpler treatment regimen for people infected with the AIDS-causing human immunodeficiency virus (HIV). Currently, HIV-infected individuals can live a near normal life span if, every day, they take a complex combination of drugs called antiretroviral therapy (ART). The bad news is if they stop ART, the small amounts of HIV that still lurk in their bodies can bounce back and infect key immune cells, called CD4 T cells, resulting in life-threatening suppression of their immune systems.
Now, a study of rhesus macaques infected with a close relative of HIV, the simian immunodeficiency virus (SIV), suggests there might be a new therapeutic option that works by a mechanism that has researchers both excited and baffled [1]. By teaming ART with a designer antibody used to treat people with severe bowel disease, NIH-funded researchers report that they have been able to keep SIV in check in macaques for at least two years after ART is stopped. More research is needed to figure out exactly how the new strategy works, and whether it would also work for humans infected with HIV. However, the findings suggest there may be a way to achieve lasting remission from HIV without the risks, costs, and inconvenience associated with a daily regimen of drugs.
Left untreated, both SIV and HIV attack and destroy CD4 T cells. Previous studies have shown that these viruses preferentially target CD4 T cells expressing high levels of a particular integrin receptor, called α4β7, on their surfaces. The receptor has also been thought to act as a kind of “zipcode” that routes CD4 T cells to the gastrointestinal tract, where they serve as a reservoir for HIV replication.
In a study published in the journal Science, researchers at Emory University School of Medicine, Atlanta, and NIH’s National Institute for Allergy and Infectious Diseases set out to explore whether response to ART might be improved by interfering with CD4 T cells that express the key integrin receptor. The agent they chose to run such interference was an antibody similar to vedolizumab, an integrin receptor-blocking antibody drug recently approved by the Food and Drug Administration for treatment of two severe intestinal diseases: ulcerative colitis and Crohn’s disease. Researchers hypothesized that this antibody might be able to prevent CD4 T cells from homing in on the gastrointestinal tract, thereby helping to control the virus better.
To test this theory, the researchers turned to the SIV-infected rhesus macaques. Eighteen macaques received daily ART treatment for about 3 months. A month into the ART regimen, 11 of the animals also began receiving infusions of an antibody similar to vedolizumab every 3 weeks and those treatments lasted about 6 months. The remaining seven animals got infusions of a non-specific antibody as a control.
As soon as the ART was stopped, SIV levels rose in the controls. In contrast, eight of the animals that received the vedolizumab-like antibody demonstrated a remarkable and lasting ability to control SIV. In fact, researchers report that levels of virus in their bloodstream have remained at low or undetectable levels for two years and counting. (An important safety note: three of the animals receiving the antibody developed immune reactions to the antibody drug, forcing their withdrawal from the study).
As you can see in the image above, the researchers used a novel PET/CT imaging technique to track CD4 T cells within the macaques. That imaging showed that the animals’ immune systems improved after the ART-antibody combo treatment. And it also revealed a big surprise: animals treated with vedolizumab-like antibody had almost normal CD4 T cell levels in their intestines. In other words, the new treatment strategy had worked—but probably not in the way the researchers had anticipated!
What’s more, SIV control in the macaques wasn’t explained by the production of broadly neutralizing antibodies (bnAbs). That is noteworthy because bnAbs are known to protect a small fraction of HIV-infected people after their immune systems have battled the virus for many years. Researchers working to develop an effective HIV vaccine have struggled for years to find ways to coax the immune system to produce those bnAbs more quickly. The new findings therefore suggest there may be another, as yet unidentified, target for HIV vaccines, as well as treatments.
It must be noted that the researchers initiated ART in the SIV-infected animals within weeks of infection, which may be difficult to achieve in HIV-infected people. If the virus was provided with additional time to take up residence in CD4 cells in the intestinal tract, the vedolizumab-like antibody might be less likely to work. Clearly, more research is needed to solve the mystery of how ART-antibody treatment acts to keep the lid on SIV over the long term, and whether it could work similarly against HIV.
We likely won’t have to wait long for more insights, however. A small, early phase human clinical trial is already underway at the NIH Clinical Center, Bethesda, MD to test whether a 30-week course of vedolizumab is safe and effective in HIV-infected volunteers. Preliminary results are expected by the end of 2017.
Reference:
[1] Sustained virologic control in SIV+ macaques after antiretroviral and α4β7 antibody therapy. Byrareddy SN, Arthos J, Cicala C, Villinger F, Ortiz KT, Little D, Sidell N, Kane MA, Yu J, Jones JW, Santangelo PJ, Zurla C, McKinnon LR, Arnold KB, Woody CE, Walter L, Roos C, Noll A, Van Ryk D, Jelicic K, Cimbro R, Gumber S, Reid MD, Adsay V, Amancha PK, Mayne AE, Parslow TG, Fauci AS, Ansari AA. Science. 2016 Oct 14;354(6309):197-202.
Links:
HIV/AIDS Basics (AIDS.gov)
HIV/AIDS (National Institute of Allergy and Infectious Diseases/NIH)
NIH Support: National Institute of Allergy and Infectious Diseases; Eunice Kennedy Shriver National Institute of Child Health and Human Development; Office of the Director
Snapshots of Life: Virus Hunting with Carbon Nanotubes

Credit: Penn State University
The purple pods that you see in this scanning electron micrograph are the H5N2 avian flu virus, a costly threat to the poultry and egg industry and, in very rare instances, a health risk for humans. However, these particular pods are unlikely to infect anything because they are trapped in a gray mesh of carbon nanotubes. Made by linking carbon atoms into a cylindrical pattern, such nanotubes are about 10,000 times smaller than width of a human hair.
The nanotubes above have been carefully aligned on a special type of silicon chip called a carbon-nanotube size-tunable-enrichment-microdevice (CNT-STEM). As described recently in Science Advances, this ultrasensitive device is designed to capture viruses rapidly based on their size, not their molecular characteristics [1]. This unique feature enables researchers to detect completely unknown viruses, even when they are present in extremely low numbers. In proof-of-principle studies, CNT-STEM made it possible to collect and detect viruses in a sample at concentrations 100 times lower than with other methods, suggesting the device and its new approach will be helpful in the ongoing hunt for new and emerging viruses, including those that infect people.
The new device is the result of a long collaboration at Penn State University, University Park, involving experts in materials science, physics, chemistry, infectious diseases, and genomics. The work was led by NIH grantees Mauricio Terrones and Si-Yang Zheng, who received additional support from an NIH Director’s New Innovator Award.
As Terrones and Zheng explained, carbon nanotubes are an ideal material to catch viruses because they are incredibly flexible and strong. They reportedly having the highest strength-to-weight ratio of any known material, which allows them to compress and bend without breaking when they encounter a virus. Another big plus is the team members can construct carbon nanotubes right on their device, controlling the distance between nanotubes with exquisite precision and, thereby, tailoring each device to the particuar size of the viruses being hunted.
To put CNT-STEM to a real-world test, Terrones and Zheng examined samples from five wild ducks in Pennsylvania, which were collected as part of a surveillance effort to track the evolution and spread of influenza viruses that could potentially cause illness in domestic poultry and/or people. They uncovered an emerging H11N9 strain of avian influenza, which couldn’t be detected by other techniques.
In a second case study, the researchers used CNT-STEM to search for viruses possibly present in a sample taken from the eyelid of a sick turkey. Earlier attempts to diagnose the turkey, which was suffering from swollen lesions of suspected viral origin, came up negative. After using the new approach to capture potential viruses in the sample, the team’s genetic analysis identified a completely novel viral strain.
CNT-STEM is lightweight and portable. It also doesn’t require any special storage, antibodies, or other chemical reagents. All of these features make it ideal for use in the field, wherever a suspected viral infection pops up. The researchers have immediate plans to work with the U.S. Department of Agriculture to apply their device in the search for viruses that may be a threat to plants, crops, and food.
It’s already feasible to make up to 1,500 of the devices per week for just a few dollars each. The next task is to scale up production, while continuing to evaluate possible refinements to the device and its technological capabilities.
Reference:
[1] Tunable and label-free virus enrichment for ultrasensitive virus detection using carbon nanotube arrays. Yeh YT, Tang Y, Sebastian A, Dasgupta A, Perea-Lopez N, Albert I, Lu H, Terrones M, Zheng SY. Sci Adv. 2016 Oct 7;2(10):e1601026.
Links:
Bird Flu (MedlinePlus, National Library of Medicine/NIH)
Terrones Research Group (Penn State University, University Park, PA)
Zheng Research Group (Penn State University, University Park, PA)
NIH Support: National Center for Advancing Translational Sciences; National Cancer Institute; Common Fund
Creative Minds: Preparing for Future Pandemics

Jonathan Abraham / Credit: ChieYu Lin
Growing up in Queens, NY, Jonathan Abraham developed a love for books and an interest in infectious diseases. One day Abraham got his hands on a copy of Laurie Garrett’s The Coming Plague, a 1990s bestseller warning of future global pandemics, and he sensed his life’s calling. He would help people around the world survive deadly viral outbreaks, particularly from Ebola, Marburg, and other really bad bugs that cause deadly hemorrhagic fevers.
Abraham, now a physician-scientist at Brigham and Women’s Hospital, Boston, continues to chase that dream. With support from an NIH Director’s 2016 Early Independence Award, Abraham has set out to help design the next generation of treatments to enable more people to survive future outbreaks of viral hemorrhagic fever. His research strategy: find antibodies in the blood of known survivors that helped them overcome their infections. With further study, he hopes to develop purified forms of the antibodies as potentially life-saving treatments for people whose own immune systems may not make them in time. This therapeutic strategy is called passive immunity.
Already, Abraham has begun collecting blood samples from survivors of Ebola, Marburg, and other hemorrhagic fevers. The next step—and it can be a long and tedious one—is to isolate the B immune cells that produce the antibodies responsible for fighting each of the viruses. When he finds one, Abraham will then identify and sequence the specific immunoglobulin genes encoding those antibodies in the appropriate B cell.
Having those DNA sequences in hand, Abraham can make large quantities of the antibodies, allowing him to study their ability to neutralize the viruses in lab dishes and infected animals. Using X-ray crystallography and cryo-electron (Cryo-EM) microscopy, he’ll also explore the structure of those antibodies in unprecedented detail.
Abraham recently reported some success in detailing the structure of the Junín virus bound to a neutralizing antibody [1]. Junín virus is endemic to north-central Argentina, where annual outbreaks occur and lead to a deadly hemorrhagic fever. It is also a virus for which transfusion of a survivor’s immune plasma—including its neutralizing antibodies—is already an established treatment. In fact, when people receive these infusions, their chances of dying from the infection drop to less than 1 percent.
Abraham hopes that structural comparisons of the protective antibodies will help to explain the inherent differences and similarities in triggering passive immunity in each of the infections under study. Knowing the similarities will point the way to promising new antibody-based treatments with potential to protect against multiple viruses. Abraham also wants to find ways to alleviate a mysterious and serious side effect of passive immunity treatment for Junín virus infection: 10 percent of treated survivors go on to develop a potentially fatal neurological syndrome, characterized by transient fevers and abnormal eye movement.
In the coming years, we can be certain that viral pandemics will continue to occur. Preparation remains vital, and Abraham and other scientists here in the United States and around the globe continue to work tirelessly to have the needed resources ready to fight the next viral pandemic.
Reference:
[1] Molecular Basis for Antibody-Mediated Neutralization of New World Hemorrhagic Fever Mammarenaviruses. Mahmutovic S, Clark L, Levis SC, Briggiler AM, Enria DA, Harrison SC, Abraham J. Cell Host Microbe. 2015 Dec 9;18(6):705-713.
Links:
Hemorrhagic Fevers (MedlinePlus/National Library of Medicine/NIH)
Jonathan Abraham (Harvard Medical School, Boston, MA)
Abraham NIH Project Information (NIH RePORTER)
NIH Director’s Early Independence Award
NIH Support: Common Fund
Twinkle, Twinkle Little Cryo-EM Star
The stars are out and shining this holiday season. But there are some star-shaped structures now under study in the lab that also give us plenty of reason for hope. One of them is a tiny virus called bacteriophage phi-6, which researchers are studying in an effort to combat a similar, but more-complex, group of viruses that can cause life-threatening dehydration in young children.
Thanks to a breakthrough technology called cryo-electron microscopy (cryo-EM), NIH researchers recently captured, at near atomic-level of detail, the 3D structure of this immature bacteriophage phi-6 particle in the process of replication. At the points of its “star,” key proteins (red) are positioned to transport clipped, single-stranded segments of the virus’ own genetic information into its newly made shell, or procapsid (blue). Once inside the procapsid, an enzyme (purple) will copy the segments to make the genetic information double-stranded, while another protein (yellow) will help package them. As the procapsid matures, it undergoes dramatic structural changes.
Because the tiny virus is easy to work with in the lab and has a genetic blueprint made of RNA, bacteriophage phi-6 has proven to be a valuable model for studying rotavirus and other more complex, double-stranded RNA viruses that make people sick.
Working in the lab of Alasdair Steven at NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases, Daniel Nemecek and Bernard Heymann produced this cryo-EM image as part of their effort to find new ways to thwart rotavirus infection, which can cause gastrointestinal upset and severe dehydration in young children. Although a vaccine is now available for the four most common strains of rotavirus, the bug still claims the lives of more than 450,000 children ages 5 and under worldwide each year, and is responsible for over 400,000 hospital visits annually in the United States alone [1]. Clearly, more must be done to prevent and treat this childhood health threat—and NIH researchers are on the case.
So, this busy holiday season, I hope you’ll join me in taking a moment to look up at the stars and reflect not only on these scientists, but the many brilliant minds around the world who are working so hard to give us the gift of better health. Happy holidays to one and all, and may this season bring you peace and joy!
Reference:
[1] Rotavirus (Centers for Disease Control and Prevention)
Links:
Developing the First Rotavirus Vaccine (Intramural Research Program/NIH)
Alasdair Steven (National Institute of Arthritis and Musculoskeletal and Skin Diseases/NIH)
NIH Support: National Institute of Arthritis and Musculoskeletal and Skin Diseases
A Lean, Mean DNA Packaging Machine

Credit: Victor Padilla-Sanchez, The Catholic University of America, Washington, D.C.
All plants and animals are susceptible to viral infections. But did you know that’s also true for bacteria? They get nailed by viruses called bacteriophages, and there are thousands of them in nature including this one that resembles a lunar lander: bacteriophage T4 (left panel). It’s a popular model organism that researchers have studied for nearly a century, helping them over the years to learn more about biochemistry, genetics, and molecular biology [1].
The bacteriophage T4 infects the bacterium Escherichia coli, which normally inhabits the gastrointestinal tract of humans. T4’s invasion starts by touching down on the bacterial cell wall and injecting viral DNA through its tube-like tail (purple) into the cell. A DNA “packaging machine” (middle and right panels) between the bacteriophage’s “head” and “tail” (green, yellow, blue spikes) keeps the double-stranded DNA (middle panel, red) at the ready. All the vivid colors you see in the images help to distinguish between the various proteins or protein subunits that make up the intricate structure of the bacteriophage and its DNA packaging machine.
Victor Padilla-Sanchez, formerly a postdoc in Venigalla Rao’s lab at The Catholic University of America, Washington, D.C., created these wonderfully detailed images. He did it by overlaying publicly available structural data for all the proteins that make up the bacteriophage T4 onto an electron micrograph image of the bacteriophage.
Then, using specialized Chimera Visualization Software on a high-performance computer, Padilla-Sanchez assembled each and every one of the bacteriophage’s approximately 2,000 proteins into this virtual 3D model. It was tedious arranging each individual protein’s crystal structure to get them to fit together just right all the way down to the atomic level. Padilla-Sanchez says it only became possible to put the final pieces together in 2015, when a team including Rao and Padilla-Sanchez solved the structure for the last of the proteins [2].
The Rao Lab wants to understand exactly how the virus and its packaging machine work and are assembled. The hope is that the bacteriophage T4 might one day be re-engineered and put to use in new treatments or vaccines for a range of health conditions, including cancer and hard-to-treat infections such as HIV.
The Rao lab already has evidence suggesting it’s possible to engineer the bacteriophage to deliver a specific antigen directly to cells of the immune system. They also envision delivering DNA encoding a toxic compound directly to cancer cells. This carefully constructed series of images, a winner in the Federation of American Societies for Experimental Biology’s 2017 BioArt competition, will be essential for that kind of future viral engineering.
References:
[1] Bacteriophage T4 genome. Miller ES, Kutter E, Mosig G, Arisaka F, Kunisawa T, Rüger W. Microbiol Mol Biol Rev. 2003 Mar;67(1):86-156.
[2] Cryo-EM structure of the bacteriophage T4 portal protein assembly at near-atomic resolution. Sun L, Zhang X, Gao S, Rao PA, Padilla-Sanchez V, Chen Z, Sun S, Xiang Y, Subramaniam S, Rao VB, Rossmann MG. Nat Commun. 2015 Jul 6;6:7548.
Links:
The Bacteriophage T4 Lab (The Catholic University of America, Washington, D.C.)
Chimera Visualization Software (University of California, San Francisco)
FASEB BioArt (Federation of American Societies for Experimental Biology, Bethesda, MD)
NIH Support: National Institute of Allergy and Infectious Diseases
Looking to Llamas for New Ways to Fight the Flu
 Researchers are making tremendous strides toward developing better ways to reduce our risk of getting the flu. And one of the latest ideas for foiling the flu—a “gene mist” that could be sprayed into the nose—comes from a most surprising source: llamas.
Researchers are making tremendous strides toward developing better ways to reduce our risk of getting the flu. And one of the latest ideas for foiling the flu—a “gene mist” that could be sprayed into the nose—comes from a most surprising source: llamas.
Like humans and many other creatures, these fuzzy South American relatives of the camel produce immune molecules, called antibodies, in their blood when exposed to viruses and other foreign substances. Researchers speculated that because the llama’s antibodies are so much smaller than human antibodies, they might be easier to use therapeutically in fending off a wide range of flu viruses. This idea is now being leveraged to design a new type of gene therapy that may someday provide humans with broader protection against the flu [1].
Scientists have had an interest in antibodies made by llamas and their camel cousins ever since their small size first was discovered about 25 years ago [2]. In fact, there are companies in Europe focused entirely on developing new treatments and technologies inspired by llama antibodies.
Recently, an international team, funded in part by NIH, has begun applying some of this fundamental knowledge about llama antibodies to our ongoing battle against the flu. In a study published in the journal Science, Joost Kolkman of Janssen Infectious Diseases, Belgium; Ian Wilson, Scripps Research Institute, La Jolla, CA; and their colleagues describe a series of experiments that have opened the door to the possibility of a new flu-fighting “gene mist.”
The work began with researchers giving llamas a fairly traditional flu shot that contained three different influenza viruses and a viral surface protein called hemagglutinin from two other viruses, representing influenza type A and B strains. Analysis of the antibodies produced by the immunized animals led to the identification of four distinct antibody types that protected against a wide range of flu viruses.
To understand better how those antibodies worked and why they could be protective against multiple strains, researchers used X-ray crystallography and cryo-electron microscopy (cryo-EM) to determine their precise molecular structures. Those studies revealed the most essential portions of the four types of antibodies for recognizing influenza viruses, each targeting a different, highly conserved location on the surface hemagglutinin of flu viruses. A conserved location is one that has been maintained through evolution, meaning the antibody’s target will be present in most viral strains, rather than changing from year to year.
Next, those antibodies were further pared down by bioengineering and the resulting “nanobodies” strung together to create a broadly protective, four-in-one antibody. Test tube studies showed that this quadruple threat effectively targets and neutralizes dozens of influenza A and B viruses, including several types of avian influenza, or bird flu.
But could this llama-derived tetravalent antibody neutralize the flu virus in living creatures? To explore that question, researchers infused the antibody directly into the bloodstreams of mice. The antibody treatment completely protected the mice against many influenza viruses that otherwise would have been deadly.
Then, with collaborators at the University of Pennsylvania, Philadelphia, the team tried a different delivery method. They designed a bioengineered gene containing the instructions for the four-in-one antibody, inserted that gene into a harmless adeno-associated virus, and sprayed that as a “gene mist” into the noses of mice. The viral vectors then inserted the genes into respiratory tract cells, which in turn produced the desired four-in-one antibody. A week later, the mice were exposed in aerosol form to various, potentially lethal influenza viruses—but they were protected.
The researchers are hopeful that a similar “gene mist” approach might provide humans with broad protection against multiple influenza strains. However, they acknowledge that such protection would gradually wear off as the cells lining the nasal passages turn over. So, depending on how long that takes, it’s possible that people would still need to get an annual flu shot.
Many questions remain to be answered before this “gene mist” approach to fending off the flu might be ready for human studies to evaluate its safety and effectiveness. Nevertheless, the strategy holds considerable promise, especially for people with fragile or compromised immune systems who may have difficulty producing their own antibodies in response to traditional flu vaccines.
And there are other intriguing possible advantages. For example, the rapid protection this approach might afford, along with its potential to neutralize many forms of avian influenza, suggest it might be called into action to help quell an emerging flu pandemic far more swiftly than is possible with traditional vaccines.
Of course, none of this is reality yet. As we look to the flu season already underway, the best way to protect yourself and your loved ones is to get your annual flu shot. So, if you’ve been procrastinating, don’t wait any longer!
References:
[1] Universal protection against influenza infection by a multidomain antibody to influenza hemagglutinin. Laursen NS, Friesen RHE, Zhu X, Jongeneelen M, Blokland S, Vermond J, van Eijgen A, Tang C, van Diepen H, Obmolova G, van der Neut Kolfschoten M, Zuijdgeest D, Straetemans R, Hoffman RMB, Nieusma T, Pallesen J, Turner HL, Bernard SM, Ward AB, Luo J, Poon LLM, Tretiakova AP, Wilson JM, Limberis MP, Vogels R, Brandenburg B, Kolkman JA, Wilson IA. Science. 2018 Nov 2;362(6414):598-602.
[2] Naturally occurring antibodies devoid of light chains. Hamers-Casterman C, Atarhouch T, Muyldermans S, Robinson G, Hamers C, Songa EB, Bendahman N, Hamers R. Nature. 1993 Jun 3;363(6428):446-448.
Links:
Wilson Lab (The Scripps Research Institute, La Jolla, CA)
Frequently Asked Flu Questions 2018-2019 Influenza Season (Centers for Disease Control and Prevention)
Influenza (National Institute of Allergy and Infectious Diseases/NIH)
Universal Influenza Vaccine Research (National Institute of Allergy and Infectious Diseases/NIH)
NIH Support: National Institute of Allergy and Infectious Diseases; National Cancer Institute; National Institute of General Medical Sciences
Enlisting CRISPR in the Quest for an HIV Cure
Today, thanks to remarkable advances in antiretroviral drugs, most people with the human immunodeficiency virus (HIV) can expect to live an almost normal lifespan. But that means staying on medications for life. If those are stopped, HIV comes roaring back in just weeks. Finding a permanent cure for HIV infection, where the virus is completely and permanently eliminated from the body, has proven much tougher. So, I’m encouraged by recent work that shows it may be possible to eliminate HIV in a mouse model, and perhaps—with continued progress—someday we will actually cure HIV in humans.
This innovative approach relies on a one-two punch: drugs and genetic editing. First, HIV-infected mice received an experimental, long-acting form of antiretroviral therapy (ART) that suppresses viral replication. This step cleared the active HIV infection. But more was needed because HIV can “hide” by inserting its DNA into its host’s chromosomes—lying dormant until conditions are right for viral replication. To get at this infectious reservoir, researchers infused the mice with a gene-editing system designed to snip out any HIV DNA still lurking in the genomes of their spleen, bone marrow, lymph nodes, and other cells. The result? Researchers detected no signs of HIV in more than one-third of mice that received the combination treatment.
The new study in Nature Communications is the product of a collaboration between the NIH-funded labs of Howard Gendelman, University of Nebraska Medical Center, Omaha, and Kamel Khalili, Temple University, Philadelphia [1]. A virologist by training, Khalili years ago realized that HIV’s ability to integrate into the genomes of its host’s cells meant that the disease couldn’t be thought of only as a typical viral infection. It had a genetic component too, suggesting that an HIV cure might require a genetic answer.
At the time, however, the tools to remove HIV DNA from human cells without harming the human genome weren’t available. That’s changed in recent years with the discovery and subsequent development of a very precise gene-editing tool known as CRISPR/Cas9.
CRISPR/Cas9 editing systems rely on a sequence-specific guide RNA to direct a scissor-like, bacterial enzyme (Cas9) to just the right spot in the genome, where it can be used to cut out, replace, or repair disease-causing mutations. Efforts are underway to apply CRISPR/Cas9 to the treatment of sickle cell disease, muscular dystrophy, and more.
Could CRISPR/Cas9 also remove HIV DNA from infected cells and eliminate the infection for good? Such an approach might be particularly helpful for people on ART who have persistent HIV DNA in the cells of their cerebrospinal fluid. A recent NIH-funded study in Journal of Clinical Investigation found that an association between this HIV reservoir and neurocognitive difficulties [2]
Earlier work by Khalili’s team showed that CRISPR could indeed remove HIV DNA from the genomes of host cells [3]. The problem was that, when delivered on its own, CRISPR couldn’t snip out every last bit of viral DNA from all cells as needed to get rid of HIV completely and permanently. It was crucial to reduce the burden of HIV genomes to the lowest possible level.
Meanwhile, Gendelman’s lab had been working to develop a new and more effective way to deliver ART. Often delivered in combinations, standard ART drugs are effective in suppressing HIV replication. However, people need to take their oral medications daily without fail. Also, most ART triple therapy drugs are water soluble, which means its cocktail of medications are swiftly processed and excreted by the body without reaching many places in the body where HIV hides.
In his quest to make ART work more effectively with fewer doses, Gendelman’s team altered the chemical composition of antiretroviral medicines, generating fat-soluble drug nanocrystals. The nanocrystals were then packaged into nanoparticles and delivered by intramuscular injection. The new drug formulation, known as long-acting slow-effective release (LASER) ART, reaches lymph nodes, spleen, gut, and brain tissues where HIV lurks [4]. Once there, it’s stored and released slowly over time. Still, like conventional ART, LASER ART can never completely cure HIV.
So, Gendelman teamed up with Khalili to ask: What would happen if LASER ART was followed by a round of CRISPR/Cas9? In a series of studies, the researchers tested LASER ART and CRISPR/Cas9, both alone and in combination. A total of 23 HIV-infected mice engineered to have some “humanized” immune features received the experimental combination therapy.
As expected, neither LASER ART nor CRISPR/Cas9 by itself proved sufficient to eradicate HIV in the mice. However, when LASER ART and CRISPR/Cas9 were delivered sequentially, the results were much different. Researchers found no evidence of HIV in the spleens or other tissues of more than one-third of the sequentially treated animals.
It’s important to note that this gene-editing approach to eradicating HIV is being applied to non-reproductive cells (somatic). The NIH does not support the use of gene-editing technologies in human embryos (germline) [5].
Of course, mice, even with humanized immune systems, are not humans. More research is needed to replicate these findings and to figure out how to make this approach to HIV treatment more effective in animal models before we can consider moving into human clinical trials. Still, these findings do provide a new reason for increased hope that an actual cure may ultimately be found for the tens of millions of people in the United States and around the globe now living with HIV.
References:
[1] Sequential LASER ART and CRISPR Treatments Eliminate HIV-1 in a Subset of Infected Humanized Mice. Dash PK, Kaminski R, Bella R, Su H, Mathews S, Ahooyi TM, Chen C, Mancuso P, Sariyer R, Ferrante P, Donadoni M, Robinson JA, Sillman B, Lin Z, Hilaire JR, Banoub M, Elango M, Gautam N, Mosley RL, Poluektova LY, McMillan J, Bade AN, Gorantla S, Sariyer IK, Burdo TH, Young WB, Amini S, Gordon J, Jacobson JM, Edagwa B, Khalili K, Gendelman HE. Nat Commun. 2019 Jul 2;10(1):2753.
[2] Spudich S et al. Persistent HIV-infected Cells in Cerebrospinal Fluid are Associated with Poorer Neurocognitive Performance. J Clin Invest. 2019. DOI: 10.1172/JCI127413 (2019).
[3] In Vivo Excision of HIV-1 Provirus by saCas9 and Multiplex Single-Guide RNAs in Animal Models. Yin C, Zhang T, Qu X, Zhang Y, Putatunda R, Xiao X, Li F, Xiao W, Zhao H, Dai S, Qin X, Mo X, Young WB, Khalili K, Hu W. Mol Ther. 2017 May 3;25(5):1168-1186.
[4] Creation of a nanoformulated cabotegravir prodrug with improved antiretroviral profiles. Zhou T, Su H, Dash P, Lin Z, Dyavar Shetty BL, Kocher T, Szlachetka A, Lamberty B, Fox HS, Poluektova L, Gorantla S, McMillan J, Gautam N, Mosley RL, Alnouti Y, Edagwa B, Gendelman HE. Biomaterials. 2018 Jan;151:53-65.
[5] Statement on Claim of First Gene-Edited Babies by Chinese Researcher. The NIH Director, NIH. 2018 November 28.
Links:
HIV/AIDS (National Institute of Allergy and Infectious Diseases/NIH)
HIV Treatment: The Basics (U.S. Department of Health and Human Services)
Fast Facts (HIV.gov)
Global Statistics (HIV.gov)
Kamel Khalili (Temple University, Philadelphia, PA)
Howard Gendelman (University of Nebraska Medical Center, Omaha)
NIH Support: National Institute of Mental Health; National Institute of Neurological Disorders and Stroke; National Institute of Allergy and Infectious Diseases; National Institute on Aging; National Institute on Drug Abuse; Common Fund
Uncovering a Hidden Zika Outbreak in Cuba

When Brazilian health officials discovered four years ago that the mosquito-borne Zika virus could cause severe birth defects and other serious health problems, it prompted a major effort across the Americas to curb the infection by controlling mosquitoes and issuing travel advisories. By mid-2017, the hard work seemed to have paid off, and reports of new Zika infections had nearly stopped.
But it turns out Zika may be tougher to control than once thought. New research shows that a large, previously hidden outbreak of Zika virus disease occurred in Cuba, just when it looked like the worst of the epidemic was over. The finding suggests that the Zika virus can linger over long periods, and that mosquito control efforts alone may slow, but not necessarily stop, the march of this potentially devastating infectious disease.
When combating global epidemics, it’s critical to track the spread of dangerous viruses from one place to the next. But some viruses can be tougher to monitor than others, and that certainly has been the case with Zika in the Americas. Though the virus can harm unborn children, many people infected with Zika never feel lousy enough to go to the doctor. Those who do often have symptoms that overlap with other prevalent tropical diseases, such as dengue and chikungunya fever, making it hard to recognize Zika.
That’s why in Brazil, where Zika arrived in the Americas by early 2014, this unexpected viral intruder went undetected for well over a year. By then, it had spread unnoticed to Honduras, circulating rapidly to other Central American nations and Mexico—likely by late 2014 and into 2015.
In the United States, even with close monitoring, a small local outbreak of Zika virus in Florida also went undetected for about three months in 2016 [1]. Then, in 2017, Florida officials began noticing something strange: new cases of Zika infection in people who had traveled to Cuba.
This came as a real surprise because Cuba, unlike most other Caribbean islands, was thought to have avoided an outbreak. What’s more, by then the Zika epidemic in the Americas had slowed to a trickle, prompting the World Health Organization to delist it as a global public health emergency of international concern.
Given the Cuban observation, some wondered whether the Zika epidemic in the Americas was really over. Among them was an NIH-supported research team, including Nathan Grubaugh, Yale School of Public Health, New Haven, CT; Sharon Isern and Scott Michael, Florida Gulf Coast University, Fort Myers; and Kristian Andersen, The Scripps Research Institute, La Jolla, CA, who worked closely with the Florida Department of Health, including Andrea Morrison.
As published in Cell, the team was able to document a previously unreported outbreak in Cuba after the epidemic had seemingly ended [2]. Interestingly, another research group in Spain also recently made a similar observation about Zika in Cuba [3].
In the Cell paper, the researchers show that between June 2017 and October 2018, all but two of 155 cases—a whopping 98 percent of travel-associated Zika infections—traced back to Cuba. Further analysis suggests that the outbreak in Cuba was likely of similar magnitude to outbreaks that occurred in other Caribbean nations.
Their estimates suggest there were likely many thousands of Zika cases in Cuba, and more than 5,000 likely should have been diagnosed and reported in 2017. The only difference was the timing. The Cuban outbreak of Zika virus occurred about a year after infections subsided elsewhere in the Caribbean.
To fill in more of the blanks, the researchers relied on Zika virus genomes from nine infected Florida travelers who returned from Cuba in 2017 and 2018. The sequencing data support multiple introductions of Zika virus to Cuba from other Caribbean islands in the summer of 2016.
The outbreak peaked about a year after the virus made its way to Cuba, similar to what happened in other places. But the Cuban outbreak was likely delayed by a year thanks to an effective mosquito control campaign by local authorities, following detection of the Brazilian outbreak. While information is lacking, including whether Zika infections had caused birth defects, it’s likely those efforts were relaxed once the emergency appeared to be over elsewhere in the Caribbean, and the virus took hold.
The findings serve as yet another reminder that the Zika virus—first identified in the Zika Forest in Uganda in 1947 and for many years considered a mostly inconsequential virus [4]—has by no means been eliminated. Indeed, such unrecognized and delayed outbreaks of Zika raise the risk of travelers innocently spreading the virus to other parts of the world.
The encouraging news is that, with travel surveillance data and genomic tools —enabled by open science—it is now possible to detect such outbreaks. By combining resources and data, it will be possible to develop even more effective and responsive surveillance frameworks to pick up on emerging health threats in the future.
In the meantime, work continues to develop a vaccine for the Zika virus, with more than a dozen clinical trials underway that pursue a variety of vaccination strategies. With the Zika pandemic resolved in the Americas, these studies can be harder to conduct, since proof of efficacy is not possible without active infections. But, as this paper shows, we must remain ready for future outbreaks of this unique and formidable virus.
References:
[1] Genomic epidemiology reveals multiple introductions of Zika virus into the United States. Grubaugh et al. Nature. 2017 Jun 15;546(7658):401-405.
[2] Travel surveillance and genomics uncover a hidden Zika outbreak during the waning epidemic. Grubaugh ND, Saraf S, Gangavarapu K, Watts A, Tan AL, Oidtman RJ, Magnani DM, Watkins DI, Palacios G, Hamer DH; GeoSentinel Surveillance Network, Gardner LM, Perkins TA, Baele G, Khan K, Morrison A, Isern S, Michael SF, Andersen .KG, et. al. Cell. 2019 Aug 22;178(5):1057-1071.e11.
[3] Mirroring the Zika epidemics in Cuba: The view from a European imported diseases clinic. Almuedo-Riera A, Rodriguez-Valero N, Camprubí D, Losada Galván I, Zamora-Martinez C, Pousibet-Puerto J, Subirà C, Martinez MJ, Pinazo MJ, Muñoz J. Travel Med Infect Dis. 2019 Jul – Aug;30:125-127.
[4] Pandemic Zika: A Formidable Challenge to Medicine and Public Health. Morens DM, Fauci AS. J Infect Dis. 2017 Dec 16;216(suppl_10):S857-S859.
Links:
Video: Uncovering Hidden Zika Outbreaks (Florida Gulf Coast University, Fort Myers)
Zika Virus (National Institute of Allergy and Infectious Diseases/NIH)
Zika Virus Vaccines (NIAID)
Zika Free Florida (Florida Department of Health, Tallahassee)
Grubaugh Lab (Yale School of Public Health, New Haven, CT)
Andersen Lab (The Scripps Research Institute, La Jolla, CA)
NIH Support: National Institute of Allergy and Infectious Diseases; National Center for Advancing Translational Sciences
How Measles Leave the Body Prone to Future Infections

As a kid who was home-schooled on a Virginia farm in the 1950s, I wasn’t around other kids very much, and so didn’t get exposed to measles. And there was no vaccine yet. Later on as a medical resident, I didn’t recognize that I wasn’t immune. So when I was hospitalized with a severe febrile illness at age 29, it took a while to figure out the diagnosis. Yes, it was measles. I have never been that sick before or since. I was lucky not to have long-term consequences, and now I’m learning that there may be even more to consider.
With the big push to get kids vaccinated, you’ve probably heard about some of the very serious complications of measles: hearing-threatening ear infections, bronchitis, laryngitis, and even life-threatening forms of pneumonia and encephalitis. But now comes word of yet another way in which the measles can be devastating—one that may also have long-term consequences for a person’s health.
In a new study in the journal Science, a research team, partly funded by NIH, found that the measles virus not only can make children deathly ill, it can cause their immune systems to forget how to ward off other common infections [1]. The virus does this by wiping out up to nearly three-quarters of the protective antibodies that a child’s body has formed in response to past microbial invaders and vaccinations. This immune “amnesia” can leave a child more vulnerable to re-contracting infections, such as influenza or respiratory syncytial virus (RSV), that they may have been protected against before they came down with measles.
The finding comes as yet another reason to feel immensely grateful that, thanks to our highly effective vaccination programs, most people born in the U.S. from the 1960s onward should never have to experience the measles.
There had been hints that the measles virus might somehow suppress a person’s immune system. Epidemiological evidence also had suggested that measles infections might lead to increased susceptibility to infection for years afterwards [2]. Scientists had even suspected this might be explained by a kind of immune amnesia. The trouble was that there wasn’t any direct proof that such a phenomenon actually existed.
In the new work, the researchers, led by Michael Mina, Tomasz Kula, and Stephen Elledge, Howard Hughes Medical Institute and Brigham and Women’s Hospital, Boston, took advantage of a tool developed a few years ago in the Elledge lab called VirScan [3]. VirScan detects antibodies in blood samples acquired as a result of a person’s past encounters with hundreds of viruses, bacteria, or vaccines, providing a comprehensive snapshot of acquired immunity at a particular moment in time.
To look for evidence of immune amnesia following the measles, the research team needed blood samples gathered from people both before and after infection. These types of samples are currently hard to come by in the U.S. thanks to the success of vaccines. By partnering with Rik de Swart, Erasmus University Medical Center, Rotterdam, Netherlands, they found the samples that they needed.
During a recent measles outbreak in the Netherlands, de Swart had gathered blood samples from children living in communities with low vaccination rates. Elledge’s group used VirScan with 77 unvaccinated kids to measure antibodies in samples collected before and about two months after their measles infections.
That included 34 children who had mild infections and 43 who had severe measles. The researchers also examined blood samples from five children who remained uninfected and 110 kids who hadn’t been exposed to the measles virus.
The VirScan data showed that the infected kids, not surprisingly, produced antibodies to the measles virus. But their other antibodies dropped and seemed to be disappearing. In fact, depending on the severity of measles infection, the kids showed on average a loss of around 40 percent of their antibody memory, with greater losses in children with severe cases of the measles. In at least one case, the loss reached a whopping 73 percent.
This all resonates with me. I do recall that after my bout with the measles, I seemed to be coming down with a lot of respiratory infections. I attributed that to the lifestyle of a medical resident—being around lots of sick patients and not getting much sleep. But maybe it was more than that.
The researchers suggest that the loss of immune memory may stem from the measles virus destroying some of the long-lived cells in bone marrow. These cells remember past infections and, based on that immunological memory, churn out needed antibodies to thwart reinvading viruses.
Interestingly, after a measles infection, the children’s immune systems still responded to new infections and could form new immune memories. But it appears the measles caused long term, possibly permanent, losses of a significant portion of previously acquired immunities. This loss of immune memory put the children at a distinct disadvantage should those old bugs circulate again.
It’s important to note that, unlike measles infection, the MMR (measles, mumps, rubella) vaccine does NOT compromise previously acquired immunity. So, these findings come as yet another reminder of the public value of measles vaccination.
Prior to 1963, when the measles vaccine was developed, 3 to 4 million Americans got the measles each year. As more people were vaccinated, the incidence of measles plummeted. By the year 2000, the disease was declared eliminated from the U.S.
Unfortunately, measles has made a come back, fueled by vaccine refusals. In October, the Centers for Disease Control and Prevention (CDC) reported an estimated 1,250 measles cases in the United States so far in 2019, surpassing the total number of cases reported annually in each of the past 25 years [4].
Around the world, measles continues to infect 7 million people each year, leading to an estimated 120,000 deaths. Based on the new findings, Elledge’s team now suspects the actual toll of the measles may be five times greater, due to the effects of immune amnesia.
The good news is those numbers can be reduced if more people get the vaccine, which has been shown repeatedly in many large and rigorous studies to be safe and effective. The CDC recommends that children should receive their first dose by 12 to 15 months of age and a second dose between the ages of 4 and 6. Older people who’ve been vaccinated or have had the measles previously should consider being re-vaccinated, especially if they live in places with low vaccination rates or will be traveling to countries where measles are endemic.
References:
[1] Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Mina MJ, Kula T, Leng Y, Li M, de Vries RD, Knip M, Siljander H, Rewers M, Choy DF, Wilson MS, Larman HB, Nelson AN, Griffin DE, de Swart RL, Elledge SJ. et al. Science. 2019 Nov 1; 366 (6465): 599-606.
[2] Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Mina MJ, Metcalf CJE, De Swart RL, Osterhaus ADME, Grenfell BT. Science. 2015 May 8; 348(6235).
[3] Viral immunology. Comprehensive serological profiling of human populations using a synthetic human virome. Xu GJ, Kula T, Xu Q, Li MZ, Vernon SD, Ndung’u T, Ruxrungtham K, Sanchez J, Brander C, Chung RT, O’Connor KC, Walker B, Larman HB, Elledge SJ. Science. 2015 Jun 5;348(6239):aaa0698.
[4] Measles cases and outbreaks. Centers for Disease Control and Prevention. Oct. 11, 2019.
Links:
Measles (MedlinePlus Medical Encyclopedia/National Library of Medicine/NIH)
Measles History (Centers for Disease Control and Prevention)
Vaccines (National Institute of Allergy and Infectious Diseases/NIAID)
Vaccines Protect Your Community (Vaccines.gov)
Elledge Lab (Harvard Medical School, Boston)
NIH Support: National Institute of Allergy and Infectious Diseases; National Institute of Diabetes and Digestive and Kidney Diseases










